Obesity is a strong risk factor for developing incontinence and several studies have suggested that weight loss may relieve urinary incontinence in obese patients and residents. In this article, you can learn more about the link between obesity and incontinence and how to treat it in everyday care.
What is Obesity?
Across the world, 13% of adults aged 18 and over are obese and 39% of adults are overweight. Worldwide obesity has nearly tripled since 1975 (9).
When we consume more energy (typically measured in calories) than the energy needed to maintain life and carry out daily activities, we gain weight. This is called an energy surplus. When we consume less energy than we need, we lose weight. This is an energy deficit (10).
This imbalance between calories consumed and calories expended is due to:
- An increased intake of high-fat foods and sugars (high-calorie foods that do not fill us up)
- An increase in physical inactivity due to a change in many forms of work, change in modes of transportation, and increased urbanization (11)
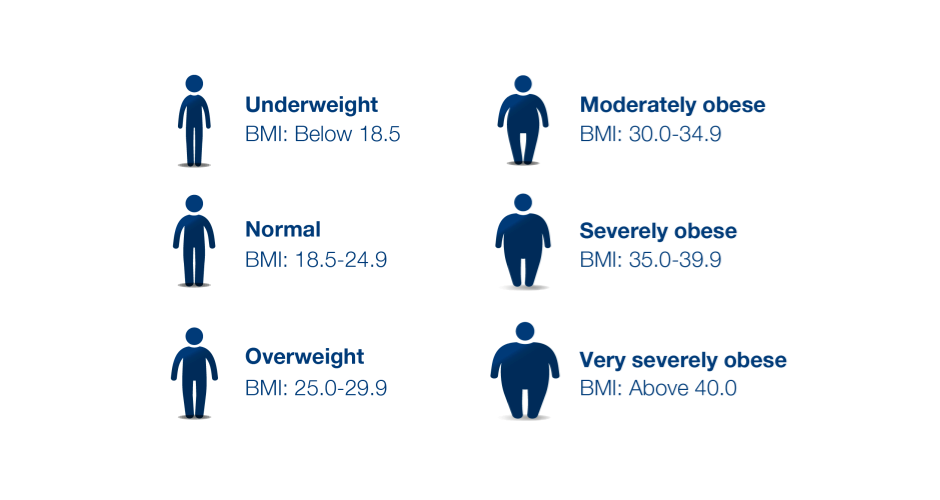
Body mass index (BMI) is the method of utilizing an adult's height and weight to broadly place them into the categories; underweight, normal weight, overweight, and obese.
BMI is a medical screening tool that estimates the amount of body fat by dividing a person's weight by the square of height in meters (m2).
How are Obesity and Incontinence Linked?
To many, it is not well-known that there is a link between obesity and urinary incontinence. However, it is convincingly verified through academic research that being overweight and having an increased BMI is associated with urinary incontinence.
This is because obesity results in increased intra-abdominal pressure. The extra fat around the belly places extra pressure on the bladder and urethra while the intra-abdominal pressure also leads to chronic stretching and strain on the pelvic floor muscle. The additional stress also results in the weakening of the pelvic floor innervation and musculature which leads to loss of control of the bladder.
Research has shown that obesity is much more common in women who live with stress and urge incontinence and especially stress incontinence is strongly associated with a BMI over 30 (2). Women should therefore know that they have a significantly increased risk of developing urinary incontinence if they are obese or overweight (3).
Types of Incontinence Associated with Obesity
Bariatric patients often live with one of two types of urinary incontinence; Stress incontinence or urge incontinence.
When there is extra pressure on the bladder it can cause residents to leak urine when sneezing, coughing, laughing,exercising, or lifting heavy objects. This is a type of incontinence called stress incontinence and is the most common type of urinary incontinence.
The extra pressure can also lead to bladder contractions resulting in the need to urinate more frequently and sometimes it’s not possible to reach the toilet in time. This type of incontinence is called urge incontinence.
However, just like everyone else, bariatric patients can also live with a combination of urge and stress incontinence. This condition is called mixed incontinence.
Working with Obese Patients
Obesity is a complex medical disease. Unfortunately, modern society has adopted negative beliefs that obese individuals are lazy, irresponsible, and lack self-discipline even though genetic, socioeconomic, and environmental factors play a large role in the development of obesity.
When treating obese residents and patients, it is important to be aware of these stigmas and to know that obese patients often come with a history of previous discrimination or embarrassment when seeking help from their healthcare provider. As a result, they may delay seeking care until they are very sick. Therefore, the state of their disease may be more advanced than for patients within the normal weight range.
Staff attitude toward caring for obese patients can easily be picked up by the patient. This can be detrimental to a patient's care, especially if the patient feels like the staff resents caring for them or is repulsed by their body habitus. Caution should be taken not to make the patient feel as if they are a spectacle or on display.
It’s also crucial in the care of people living with obesity and incontinence to focus on the condition of the skin.
Potential Skin Issues for Obese People Living with Incontinence
Skin problems such as chronic wounds, lymphedema, intertrigo, diabetic foot ulcers, incontinence-associated dermatitis (IAD), and more, are common in bariatric patients (5).
Skinfolds due to obesity is warm and moist and ideal for microorganism growth. Here it is important to avoid tight clothes and use a pH -balanced cleansing product and pat skinfolds dry rather than rubbing. Genital and perineal skin can be especially challenging to care for patients who are obese. They may have deep skin folds in the groin and buttock area, which are exposed to high friction and increased moisture from urinary incontinence and perspiration. Perineal care requires carefully assessing these areas while respecting a patient’s modesty and comfort.
Further, hygiene after toileting can be challenging for patients who are obese, increasing the risk of skin breakdown or infection in the genital and perineal area. Washcloths or premoistened wipes can be preferable to toilet paper and using a handheld showerhead when bathing may aid hygiene. Using a wet wash wipe is also a great alternative.
Caring for Bariatric Skin
When caring for bariatric skin, we recommend following our three-step process; 1) breathable protection, 2) gentle cleansing, and 3) moisture and barrier.
Proper skincare starts with the right incontinence product, that lets the skin breathe while having an absorbency that is suitable for the resident’s needs. If you need help finding the right product, try our incontinence product selector.
Cleaning and drying the skin gently but thoroughly and applying barrier products after every voiding is highly recommended to protect vulnerable skin.
When changing the incontinence product, we recommend using wash-without-water products that are suitable for fragile skin. For instance, using a wash glove and washing foam combination can make it easier for staff to feel their way during perineal care while easing the work process of cleaning the perineal area, as no soap and water are needed.
Barrier products are intended to protect the skin from urine and feces, preventing irritation and redness, while also hydrating the skin to keep it soft and moisturized. This helps reduce the risk of cracking and infection. At the same time, barrier products are formulated to help defend the skin against bacteria.
Gently patting the product on is preferable to rubbing in the cream, as you minimize the risk of causing friction that can damage the skin. When using an incontinence product, too thick a layer of barrier cream on the skin can impair the absorption of the brief and result in leakages. At the same time, too much product can also cause skin cracking and discomfort.
In some cases, using a zinc spray rather than a cream or ointment can be beneficial. A spray is easier to apply and doesn’t require any rubbing on fragile skin. We recommend using our Zinc Spray with 10% zinc oxide as it absorbs quickly into the skin and doesn’t require that you wipe any excess product off.
Treatment Options
Though incontinence is not a harmful condition, it can profoundly affect residents' quality of life due to physical and emotional discomfort. However, depending on the type of incontinence, bladder muscle training, pharmacologic treatments, and weight loss are among some of the treatment options.
Studies have shown that weight loss between 5% and 10% of the total body weight will be sufficient for significant urinary incontinence relief. Thus, weight loss should be considered the initial treatment for incontinence in overweight and obese people.
Studies have shown that with a behavioral weight-loss program there is a significantly greater reduction in urinary incontinence episodes. In obese women living with stress incontinence, a reduction in weight at 8% in 6 months has proven to decrease urinary incontinence episodes by 70%. Weight loss will also reduce the risk of developing obesity complications and co-diseases (8).
However, research shows that weight stigma leads to adverse physical and psychological consequences for people living with obesity. Studies have shown that people internalize the stigma and are less confident in their ability to lose weight, leading to behaviors such as binge eating and reduced activity level.
To aid a resident or patient in weight loss it is important to take a holistic approach and consider potential comorbidities (see next section). It is not enough to simply cut down calories, as severe obesity can have many underlying reasons such as psychological, medical, metabolic, and much more.
Therefore, always consult with a doctor and dietitian before starting a treatment plan focused on weight loss.
Obesity and Other Risk Factors
People living with obesity, are not only predisposed to incontinence. Obesity can also lead to an increased risk of developing comorbidities. Which diseases a person will develop, among other things, depends on factors such as physical activity level, diet composition, and genes that increase the risk of insulin resistance and type 2 diabetes. The risk is significantly increased when a person’s BMI is over 30.
Here are some of the complications obese people are at risk of developing (6):
- Cardiovascular disease
- Coronary heart disease
- Stroke
- Type 2 diabetes
- Gastrointestinal and hepatobiliary complications
- Cancer
- Gallbladder disease
- Obstructive sleep apnea
- Asthma
- Osteoarthritis
- Anxiety
Additionally, weight stigma leads to a greater risk of depression, suicidal ideation, and low self-esteem (7). As such, obesity is a complex matter and it is necessary to take a holistic approach when treating it.